Efficacy of Intranasal Dexmedetomidine as a Preoperative Anxiolytic in Children: A Systematic Review
DOI:
https://doi.org/10.18776/72vx2g19Keywords:
dexmedetomidine, premedication, anxiety, intranasal, childrenAbstract
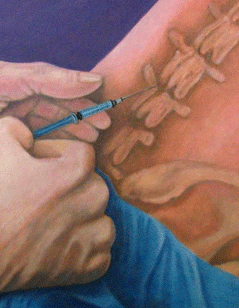
Preoperative anxiety is a common problem in pediatric patients that can have many negative effects; oral premedications (eg, midazolam) are often used to reduce anxiety and improve compliance. Dexmedetomidine (DEX) is an alpha-2 receptor agonist that can be given intranasally to children as a premedication and may be useful as an anxiolytic. In this systematic review of the PubMed, CINAHL, Ovid, and Cochrane Library databases, the efficacy of intranasal dexmedetomidine (IN DEX) was compared with that of oral midazolam for relieving preoperative anxiety among pediatric surgical patients. Three trials were assessed: 2 of these trials concluded that IN DEX was a superior anxiolytic for use in children; the third showed that there was no significant difference. More rigorous research that includes a larger sample size and an objective measurement tool is needed before drawing conclusions.
References
Kain ZN, Mayes LC, O'Connor TZ, Cicchetti DV. Preoperative anxiety in children. predictors and outcomes. Arch Pediatr Adolesc Med. 1996;150(12):1238-1245.
Kain ZN, Mayes LC, Caldwell-Andrews AA, Karas DE, McClain BC. Preoperative anxiety, postoperative pain, and behavioral recovery in young children undergoing surgery. Pediatrics. 2006;118(2):651-658.
Fortier MA, Del Rosario AM, Martin SR, Kain ZN. Perioperative anxiety in children. Paediatr Anaesth. 2010;20(4):318-322.
Strom S. Preoperative evaluation, premedication, and induction of anesthesia in infants and children. Curr Opin Anaesthesiol. 2012;25(3):321-325.
Kain ZN, Caldwell-Andrews AA, Krivutza DM, Weinberg ME, Wang SM, Gaal D. Trends in the practice of parental presence during induction of anesthesia and the use of preoperative sedative premedication in the united states, 1995-2002: Results of a follow-up national survey. Anesth Analg. 2004;98(5):9, table of contents.
Kain ZN, Mayes LC, Bell C, Weisman S, Hofstadter MB, Rimar S. Premedication in the united states: A status report. Anesth Analg. 1997;84(2):427-432.
Almenrader N, Passariello M, Coccetti B, Haiberger R, Pietropaoli P. Premedication in children: A comparison of oral midazolam and oral clonidine. Paediatr Anaesth. 2007;17(12):1143-1149.
Kogan A, Katz J, Efrat R, Eidelman LA. Premedication with midazolam in young children: A comparison of four routes of administration. Paediatr Anaesth. 2002;12(8):685-689.
Bergendahl H, Lonnqvist PA, Eksborg S. Clonidine in paediatric anaesthesia: Review of the literature and comparison with benzodiazepines for premedication. Acta Anaesthesiol Scand. 2006;50(2):135-143.
Primosch RE, Bender F. Factors associated with administration route when using midazolam for pediatric conscious sedation. ASDC J Dent Child. 2001;68(4):8, 228.
Jia JE, Chen JY, Hu X, Li WX. A randomised study of intranasal dexmedetomidine and oral ketamine for premedication in children. Anaesthesia. 2013;68(9):944-949.
Devabhakthuni S, Pajoumand M, Williams C, Kufera JA, Watson K, Stein DM. Evaluation of dexmedetomidine: Safety and clinical outcomes in critically ill trauma patients. J Trauma. 2011;71(5):1164-1171.
Yao Y, Qian B, Lin Y, Wu W, Ye H, Chen Y. Intranasal dexmedetomidine premedication reduces minimum alveolar concentration of sevoflurane for laryngeal mask airway insertion and emergence delirium in children: A prospective, randomized, double-blind, placebo-controlled trial. Paediatr Anaesth. 2015;25(5):492-498.
Abdelaziz HMM, Bakr RH, Kasem AA. Effect of intranasal dexmedetomidine or intranasal midazolam on prevention of emergence agitation in pediatric strabismus surgery: A randomized controlled study. Egyptian Journal of Anaesthesia. 2016;32(3):285-291. doi: 10.1016/j.egja.2015.11.009.
Sheta SA, Al-Sarheed MA, Abdelhalim AA. Intranasal dexmedetomidine vs midazolam for premedication in children undergoing complete dental rehabilitation: A double-blinded randomized controlled trial. Paediatr Anaesth. 2014;24(2):181-189.
Chokshi AA, Patel VR, Chauhan PR, Patel DJ, Chadha IA, Ramani MN. Evaluation of intranasal midazolam spray as a sedative in pediatric patients for radiological imaging procedures. Anesth Essays Res. 2013;7(2):189-193.
Iirola T, Vilo S, Manner T, et al. Bioavailability of dexmedetomidine after intranasal administration. Eur J Clin Pharmacol. 2011;67(8):825-831.
Daabiss M. American society of anaesthesiologists physical status classification. Indian journal of anaesthesia. 2011;55(2):111-115. http://www.ncbi.nlm.nih.gov/pubmed/21712864. doi: 10.4103/0019-5049.79879.
Yuen VM, Hui TW, Irwin MG, Yuen MK. A comparison of intranasal dexmedetomidine and oral midazolam for premedication in pediatric anesthesia: A double-blinded randomized controlled trial. Anesth Analg. 2008;106(6):1715-1721.
Ghali AM, Mahfouz AK, Al-Bahrani M. Preanesthetic medication in children: A comparison of intranasal dexmedetomidine versus oral midazolam. Saudi J Anaesth. 2011;5(4):387-391.
Linares Segovia B, Garcia Cuevas MA, Ramirez Casillas IL, et al. Pre-anesthetic medication with intranasal dexmedetomidine and oral midazolam as an anxiolytic. A clinical trial. An Pediatr (Barc). 2014;81(4):226-231.
Kain ZN, Mayes LC, Cicchetti DV, Bagnall AL, Finley JD, Hofstadter MB. The yale preoperative anxiety scale: How does it compare with a "gold standard"? Anesth Analg. 1997;85(4):783-788.
James T Croasmun, Lee Ostrom. Using likert-type scales in the social sciences. Journal of Adult Education. 2011;40(1):19. http://search.proquest.com/docview/1018567864.
MacLaren JE, Hammell C, Novoa C, Mednick L, Kain ZN. How much time do we spend in preoperative holding: Findings of a video capture system. Anesthesiology. 2007;107.
Kain ZN, MacLaren JE, Hammell C, et al. Healthcare provider-child-parent communication in the preoperative surgical setting. Paediatr Anaesth. 2009;19(4):376-384.
Downloads
Published
Issue
Section
License
Authors agree to the Creative Commons License listed below, which can be viewed by clicking the link below.
This work will be licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.